
The relationship between sleep and many important health outcomes is well established. From practicing good sleep hygiene to tracking sleep phases using smartwatches, many Americans are spending more of their waking hours thinking about the quality and quantity of their sleep. However, one aspect of sleep health that’s often overlooked is how age-related changes can impact both the experience and measurement of sleep. The relationship between aging and sleep is especially important given the role that sleep serves in clearing waste from the brain—a process that may be essential to preserving cognitive function.
In a MassAITC Webinar Series talk delivered on June 28, 2022, Dr. Rebecca Spencer, professor of psychological and brain sciences and sleep lab facilities director at the University of Massachusetts Amherst, outlines current challenges and opportunities in sleep measurement, highlighting important considerations for researchers and device designers studying sleep in older adults.
Sleeping and aging well
Sleep impacts physical, mental, and cognitive well-being throughout the lifespan, and may be associated with important physical and cognitive outcomes for older adults. During sleep, the brain can consolidate memories, assist in decision-making, engage in emotion regulation, and activate the glymphatic system to clear waste from the brain—including amyloid beta and tau proteins, which researchers have linked to the progression of Alzheimer’s disease and related dementias (AD/ADRD). Dr. Spencer notes that high-quality sleep can become more difficult with age due to a host of physical, mental, and environmental changes. Factors such as weight, hormones, ambient light or sound, bed partners, and mental disorders can decrease the quality of sleep. Therefore, studying sleep throughout the aging process and in the presence of mental or other cognitive disorders is highly important.
Sizing up sleep
The gold-standard approach to studying sleep is polysomnography, in which electrodes placed on the head measure factors such as brain activity, eye movements, and muscle movements. Recording these throughout sleep allow researchers to identify sleep stages and their duration. Dr. Spencer explains that polysomnography currently provides the largest array of data and allows for increased accuracy and specificity when performing sleep studies. However, these data come at a price. Polysomnography equipment is time consuming to apply correctly, requires hours of data review to identify sleep stages, and is best applied in a controlled laboratory setting. Additionally, polysomnography equipment can be highly uncomfortable for patients and may impact sleep while patients acclimate to the equipment. These constraints can limit the number of participants studied and reduce the feasibility of using polysomnography to study sleep in non-laboratory settings, such as among older adults aging at home.

Actigraphy devices—wearable activity monitors that identify sleep through periods of low to no activity—offer a more versatile, if less intensive, alternative to polysomnography. These devices are commercially available from consumer brands including FitBit, Oura, and Samsung. Some devices utilize additional features to capture data regarding pulse, oximetry, temperature, and more to identify and track sleep. These devices are much smaller than polysomnography equipment, can often be worn as a watch or a ring, and are typically more comfortable for people to wear while sleeping. This can allow researchers to capture data over multiple days and in non-laboratory settings while minimally interrupting sleep habits.
However, Dr. Spencer notes that actigraphy is not without fault. Sensors that monitor temperature, pulse, and oximetry cannot replace the wealth of precise sleep data that polysomnography captures through brain wave monitoring. Instead, actigraphy devices typically use algorithms to make a best guess for sleep and wake onset and are unable to determine specific sleep stages. These algorithms are not always made available to researchers, further obscuring the data available and their interpretation.
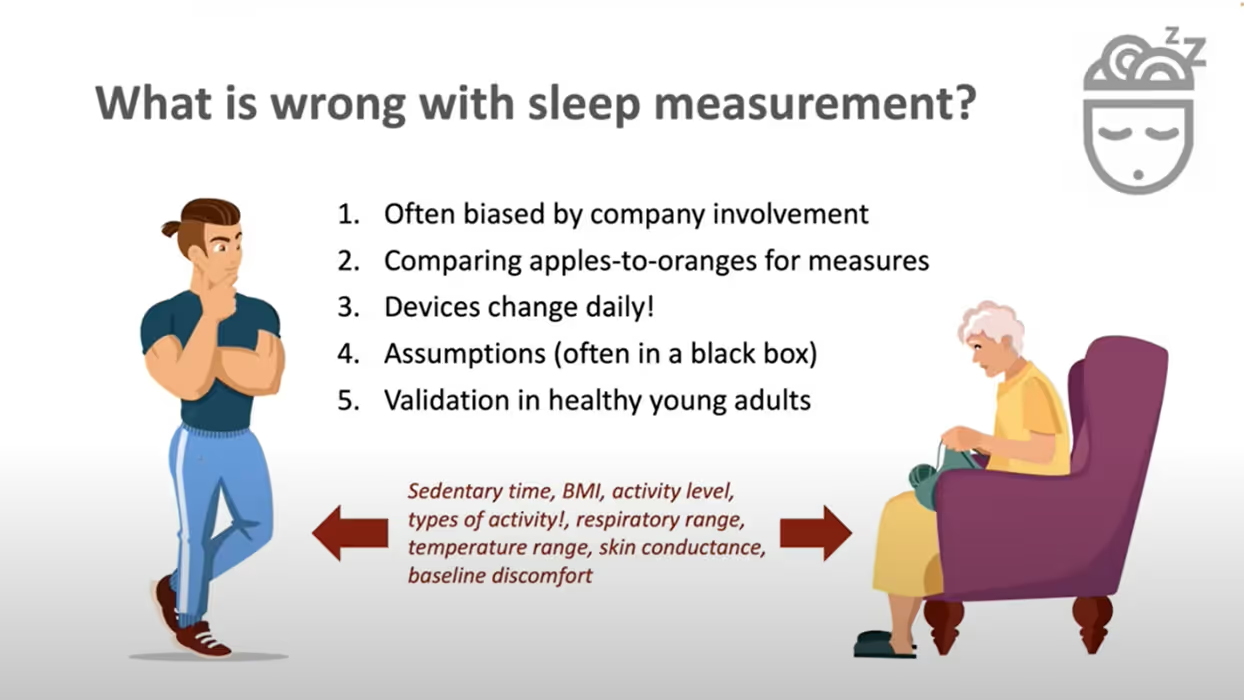
Furthermore, actigraphy may be suboptimal for studying sleep in older adults when devices are not designed with that population in mind. Device validation often utilizes healthy young adults and may not account for older populations, physical disorders, or mental decline. Algorithms designed for and validated in young adult populations are unlikely to account for older adults’ highly variable vital signs and activity levels. The fit of actigraphy devices may be uncomfortable on thinner, aging skin or exacerbate agitation experienced by those with AD/ADRD. In addition, interacting with a device to input supplementary data such as exercise, ambient lighting, or diet may be challenging for users who lack technical experience or are experiencing cognitive decline.
Improved measures for better sleep health
Dr. Spencer emphasizes the importance of carefully considering the devices that will be utilized when designing a sleep study. Factors to consider include not only the quality and quantity of data generated, but also whether the device used is appropriate to the lifestyle of individual participants and whether device algorithms are applicable to the population of interest. Currently, polysomnography is the only method capable of determining specific sleep phases, but it is limited by cost, processing hours, and potential impact on a patient’s normal sleep. Actigraphy is far less intrusive and requires fewer processing hours but does not capture differences in sleep phases and often has not been validated for older adults or those experiencing physical, mental, or cognitive disorders.
The benefits and drawbacks of each of these approaches to measuring sleep inform important avenues for future study. Dr. Spencer encourages studies that seek to validate actigraphy devices in populations including older adults and individuals with AD/ADRD. Additionally, advances in sleep study technology should seek to combine the comfort and unobtrusiveness of actigraphy with the wealth of data provided by polysomnography. Developments that reduce the size and quantity of electrodes required to capture brain waves would revolutionize sleep studies, with the potential to accelerate insights and innovations to improve the sleep and health of older adults.
Dr. Rebecca Spencer is a professor in the Department of Psychological and Brain Sciences and the director of the Institute for Applied Life Sciences Sleep Monitoring Lab at the University of Massachusetts Amherst. View Dr. Spencer’s full talk here and learn more about MassAITC at massaitc.org.




